Tuberculosis or TB (short for tubercles bacillus) is a common and often deadly infectious disease caused by various strains of mycobacteria, usually Mycobacterium tuberculosis in humans. Tuberculosis usually attacks the lungs but can also affect other parts of the body. It is spread through the air, when people who have the disease cough, sneeze, or spit. Most infections in humans result in an asymptomatic, latent infection, and about one in ten latent infections eventually progresses to active disease, which, if left untreated, kills more than 50% of its victims.
The classic symptoms are a chronic cough with blood-tinged sputum, fever, night sweats, and weight loss. Infection of other organs causes a wide range of symptoms. Diagnosis relies on radiology (commonly chest X-rays), a tuberculin skin test, blood tests, as well as microscopic examination and microbiological culture of bodily fluids. Treatment is difficult and requires long courses of multiple antibiotics. Contacts are also screened and treated if necessary. Antibiotic resistance is a growing problem in (extensively) multi-drug-resistant tuberculosis. Prevention relies on screening programs and vaccination, usually with Bacillus Calmette-Guérin vaccine.
A third of the world's population are thought to be infected with M. tuberculosis, and new infections occur at a rate of about one per second.The proportion of people who become sick with tuberculosis each year is stable or falling worldwide but, because of population growth, the absolute number of new cases is still increasing. In 2007 there were an estimated 13.7 million chronic active cases, 9.3 million new cases, and 1.8 million deaths, mostly in developing countries. In addition, more people in the developed world are contracting tuberculosis because their immune systems are compromised by immunosuppressive drugs, substance abuse, or AIDS. The distribution of tuberculosis is not uniform across the globe; about 80% of the population in many Asian and African countries test positive in tuberculin tests, while only 5-10% of the US population test positive.
Classification
Main article: Tuberculosis classification
The current clinical classification system for tuberculosis (TB) is based on the pathogenesis of the disease.[citation needed]
| Class | Type | Description |
|---|---|---|
| 0 | No TB exposure Not infected | No history of exposure Negative reaction to tuberculin skin test |
| 1 | TB exposure No evidence of infection | History of exposure Negative reaction to tuberculin skin test Ghon complex |
| 2 | TB infection No disease | Positive reaction to tuberculin skin test Negative bacteriologic studies (if done) Fibrocaseous cavitary lesion (usually in upper lobe of lungs) |
| 3 | TB, clinically active | M. tuberculosis cultured (if done) Clinical, bacteriologic, or radiographic evidence of current disease |
| 4 | TB Not clinically active | History of episode(s) of TB or Abnormal but stable radiographic findings Positive reaction to the tuberculin skin test Negative bacteriologic studies (if done) and No clinical or radiographic evidence of current disease |
| 5 | TB suspect | Diagnosis pending TB disease should be ruled in or out within 3 months |
Signs and symptoms
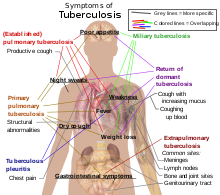
When the disease becomes active, 75% of the cases are pulmonary TB, that is, TB in the lungs. Symptoms include chest pain, coughing up blood, and a productive, prolonged cough for more than three weeks. Systemic symptoms include fever, chills, night sweats, appetite loss, weight loss, pallor, and often a tendency to fatigue very easily.
In the other 25% of active cases, the infection moves from the lungs, causing other kinds of TB, collectively denoted extrapulmonary tuberculosis. This occurs more commonly in immunosuppressed persons and young children. Extrapulmonary infection sites include the pleura in tuberculosis pleurisy, the central nervous systemmeningitis, the lymphatic system in scrofula of the neck, the genitourinary system in urogenital tuberculosis, and bones and joints in Pott's disease of the spine. An especially serious form is disseminated TB, more commonly known as miliary tuberculosis. Extrapulmonary TB may co-exist with pulmonary TB as well. in
Causes
Main article: Mycobacterium tuberculosis
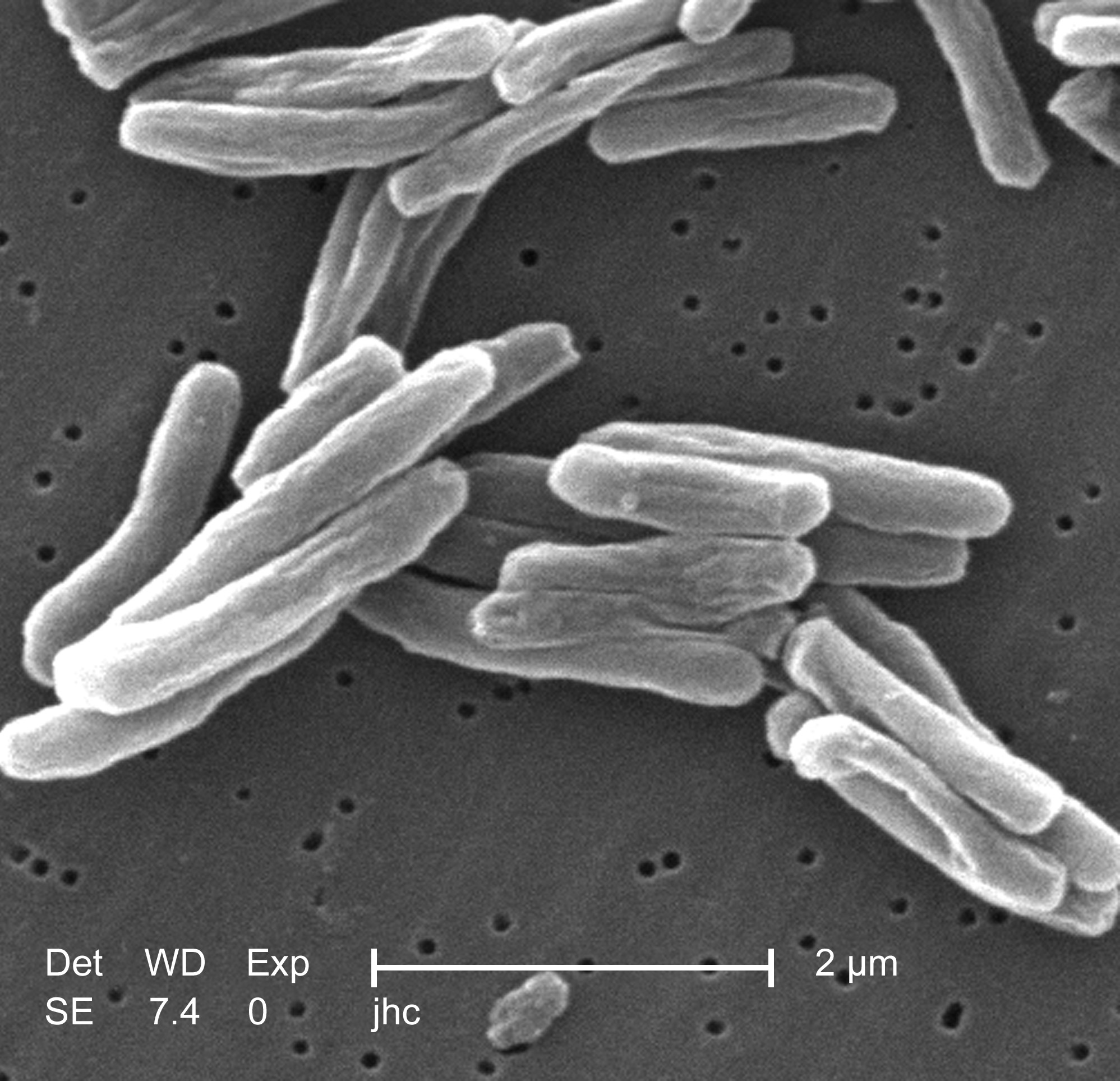
The primary cause of TB, Mycobacterium tuberculosis, is a small aerobic non-motile bacillus. High lipid[10] It divides every 16 to 20 hours, an extremely slow rate compared with other bacteria, which usually divide in less than an hour. (For example, one of the fastest-growing bacteria is a strain of E. coli that can divide roughly every 20 minutes.) Since MTB has a cell wall but lacks a phospholipid outer membrane, it is classified as a Gram-positiveGram stain is performed, MTB either stains very weakly Gram-positive or does not retain dye due to the high lipid & mycolic acid content of its cell wall. MTB can withstand weak disinfectantsdry state for weeks. In nature, the bacterium can grow only within the cells of a hostM. tuberculosis can be cultured in vitro. content of this pathogen accounts for many of its unique clinical characteristics. bacterium. However, if a and survive in a organism, but
Using histological stains on expectorate samples from phlegm (also called sputum), scientists can identify MTB under a regular microscope. Since MTB retains certain stains after being treated with acidic solution, it is classified as an acid-fast bacillus (AFB). The most common acid-fast staining technique, the Ziehl-Neelsen stain, dyes AFBs a bright red that stands out clearly against a blue background. Other ways to visualize AFBs include an auramine-rhodamine stain and fluorescent microscopy.
The M. tuberculosis complex includes four other TB-causing mycobacteria: M. bovis, M. africanum, M. canetti and M. microti. M. africanum is not widespread, but in parts of Africa it is a significant cause of tuberculosis. M. bovis was once a common cause of tuberculosis, but the introduction of pasteurized milk has largely eliminated this as a public health problem in developed countries. M. canetti is rare and seems to be limited to Africa, although a few cases have been seen in African emigrants. M. microti is mostly seen in immunodeficient people, although it is possible that the prevalence of this pathogen has been underestimated.
Other known pathogenic mycobacteria include Mycobacterium leprae, Mycobacterium avium and M. kansasii. The last two are part of the nontuberculous mycobacteria (NTM) group. Nontuberculous mycobacteria cause neither TB nor leprosy, but they do cause pulmonary diseases resembling TB.
Risk factors
Persons with silicosis have an approximately 30-fold greater risk for developing TB. Silica particles irritate the respiratory system, causing immunogenic responses such as phagocytosis which consequently results in high lymphatic vessel deposits. It is this interference and blockage of macrophage function which increases the risk of tuberculosis. Persons with chronic renal failure who are on hemodialysis also have an increased risk: 10—25 times greater than the general population. Persons with diabetes mellitus have a risk for developing active TB that is two to four times greater than persons without diabetes mellitus, and this risk is likely greater in persons with insulin-dependent or poorly controlled diabetes. Other clinical conditions that have been associated with active TB include gastrectomy with attendant weight loss and malabsorption, jejunoileal bypass, renal and cardiac transplantation, carcinoma of the head or neck, and other neoplasms (e.g., lung cancer, lymphoma, and leukemia).
Given that silicosis greatly increases the risk of tuberculosis, more research about the effect of various indoor or outdoor air pollutants on the disease would be necessary. Some possible indoor source of silica includes paint, concrete and Portland cement. Crystalline silica is found in concrete, masonry, sandstone, rock, paint, and other abrasives. The cutting, breaking, crushing, drilling, grinding, or abrasive blasting of these materials may produce fine silica dust. It can also be in soil, mortar, plaster, and shingles. When you wear dusty clothing at home or in your car, you may be carrying silica dust that your family will breathe.
Low body weight is associated with risk of tuberculosis as well. A body mass index (BMI) below 18.5 increases the risk by 2—3 times. On the other hand, an increase in body weight lowers the risk. Patients with diabetes mellitus are at increased risk of contracting tuberculosis, and they have a poorer response to treatment, possibly due to poorer drug absorption
Other conditions that increase risk include IV drug abuse; recent TB infection or a history of inadequately treated TB; chest X-ray suggestive of previous TB, showing fibrotic lesions and nodules; prolonged corticosteroid therapy and other immunosuppressive therapy; Immunocompromised patients (30-40% of AIDS patients in the world also have TB) hematologic and reticuloendothelial diseases, such as leukemia and Hodgkin's disease; end-stage kidney disease; intestinal bypass; chronic malabsorption syndromes; vitamin D deficiency; and low body weight
Twin studies in the 1940s showed that susceptibility to TB was heritable. If one of a pair of twins got TB, then the other was more likely to get TB if he was identical than if he was not. These findings were more recently confirmed by a series of studies in South Africa. Specific gene polymorphisms in IL12B have been linked to tuberculosis susceptibility.
Some drugs, including rheumatoid arthritis drugs that work by blocking tumor necrosis factor-alpha (an inflammation-causing cytokine), raise the risk of activating a latent infection due to the importance of this cytokine in the immune defense against TB.
Mechanism
Transmission
When people suffering from active pulmonary TB cough, sneeze, speak, or spit, they expel infectious aerosolµm in diameter. A single sneeze can release up to 40,000 droplets. Each one of these droplets may transmit the disease, since the infectious dose of tuberculosis is very low and inhaling less than ten bacteria may cause an infection. droplets 0.5 to 5
People with prolonged, frequent, or intense contact are at particularly high risk of becoming infected, with an estimated 22% infection rate. A person with active but untreated tuberculosis can infect 10–15 other people per year. Others at risk include people in areas where TB is common, people who inject drugs using unsanitary needles, residents and employees of high-risk congregate settings, medically under-served and low-income populations, high-risk racial or ethnic minority populations, children exposed to adults in high-risk categories, patients immunocompromised by conditions such as HIV/AIDS, people who take immunosuppressant drugs, and health care workers serving these high-risk clients.
Transmission can only occur from people with active — not latent — TB . The probability of transmission from one person to another depends upon the number of infectious droplets expelled by a carrier, the effectiveness of ventilation, the duration of exposure, and the virulence of the M. tuberculosis strain. The chain of transmission can, therefore, be broken by isolating patients with active disease and starting effective anti-tuberculous therapy. After two weeks of such treatment, people with non-resistant active TB generally cease to be contagious. If someone does become infected, then it will take at least 21 days, or three to four weeks, before the newly infected person can transmit the disease to others.TB can also be transmitted by eating meat infected with TB. Mycobacterium bovis causes TB in cattle. (See details below.)
Pathogenesis
About 90% of those infected with Mycobacterium tuberculosis have asymptomatic, latent TB infection (sometimes called LTBI), with only a 10% lifetime chance that a latent infection will progress to TB disease. However, if untreated, the death rate for these active TB cases is more than 50%.
TB infection begins when the mycobacteria reach the pulmonary alveoli, where they invade and replicate within the endosomes of alveolar macrophages. The primary site of infection in the lungs is called the Ghon focus, and is generally located in either the upper part of the lower lobe, or the lower part of the upper lobe.dendritic cells, which do not allow replication, although these cells can transport the bacilli to local (mediastinal) lymph nodes. Further spread is through the bloodstream to other tissues and organs where secondary TB lesions can develop in other parts of the lung (particularly the apex of the upper lobes), peripheral lymph nodes, kidneys, brain, and bone. All parts of the body can be affected by the disease, though it rarely affects the heart, skeletal muscles, pancreas and thyroid. Bacteria are picked up by
Tuberculosis is classified as one of the granulomatous inflammatory conditions. Macrophages, T lymphocytes, B lymphocytes and fibroblasts are among the cells that aggregate to form a granuloma, with lymphocytescytokines such as interferon gamma, which activates macrophages to destroy the bacteria with which they are infected.Cytotoxic T cells can also directly kill infected cells, by secreting perforin and granulysin. surrounding the infected macrophages. The granuloma functions not only to prevent dissemination of the mycobacteria, but also provides a local environment for communication of cells of the immune system. Within the granuloma, T lymphocytes secrete
Importantly, bacteria are not always eliminated within the granuloma, but can become dormant, resulting in a latent infection Another feature of the granulomas of human tuberculosis is the development of abnormal cell death, also called necrosis, in the center of tubercles. To the naked eye this has the texture of soft white cheese and was termed caseous necrosis.
If TB bacteria gain entry to the bloodstream from an area of damaged tissue they spread through the body and set up many foci of infection, all appearing as tiny white tubercles in the tissues. This severe form of TB disease is most common in infants and the elderly and is called miliary tuberculosis. Patients with this disseminated TB have a fatality rate near 100% if untreated. However, If treated early, the fatality rate is reduced to near 10%.
In many patients the infection waxes and wanes. Tissue destruction and necrosis are balanced by healing and fibrosis. Affected tissue is replaced by scarring and cavities filled with cheese-like white necrotic material. During active disease, some of these cavities are joined to the air passages bronchi and this material can be coughed up. It contains living bacteria and can therefore pass on infection. Treatment with appropriate antibiotics kills bacteria and allows healing to take place. Upon cure, affected areas are eventually replaced by scar tissue.
If untreated, infection with Mycobacterium tuberculosis can become lobar pneumonia.
Diagnosis
For more details on this topic, see Tuberculosis diagnosis.
Tuberculosis is diagnosed definitively by identifying the causative organism (Mycobacterium tuberculosis) in a clinical sample (for example, sputum or pus). When this is not possible, a probable - although sometimes inconclusive - diagnosis may be made using imaging (X-rays or scans) and/or a tuberculin skin test (Mantoux test).
The main problem with tuberculosis diagnosis is the difficulty in culturing this slow-growing organism in the laboratory (it may take 4 to 12 weeks for blood or sputum culture). A complete medical evaluation for TB must include a medical history, a physical examination, a chest X-ray, microbiological smears, and cultures. It may also include a tuberculin skin test, a serological test. The interpretation of the tuberculin skin test depends upon the person's risk factors for infection and progression to TB disease, such as exposure to other cases of TB or immunosuppression.
Currently, latent infection is diagnosed in a non-immunized person by a tuberculin skin test, which yields a delayed hypersensitivity type response to an extract made from M. tuberculosis. Those immunized for TB or with past-cleared infection will respond with delayed hypersensitivity parallel to those currently in a state of infection, so the test must be used with caution, particularly with regard to persons from countries where TB immunization is common. Tuberculin tests have the disadvantage of producing false negatives, especially when the patient is co-morbid with sarcoidosis, Hodgkins lymphoma, malnutrition, or most notably active tuberculosis disease The newer interferon release assays (IGRAs) overcome many of these problems. IGRAs are in vitro blood tests that are more specific than the skin test. IGRAs detect the release of interferon gamma in response to mycobacterial proteins such as ESAT-6. These are not affected by immunization or environmental mycobacteria, so generate fewer false positive results. There is also evidence that the T-SPOT.TB IGRA is more sensitive than the skin test[. Diagnosis of TB has also been done with use of various radiotracers using nuclear medicine methods, which not only detects but also locates tubercular infection .
New TB tests are being developed that offer the hope of cheap, fast and more accurate TB testing. These include polymerase chain reaction assays for the detection of bacterial DNA. The development of a rapid and inexpensive diagnostic test would be particularly valuable in the developing world..
Prevention

Map showing the 22 high-burden countries (HBC) that according to WHO account for 80% of all new TB cases arising each year. The Global Plan is especially aimed at these countries.
TB prevention and control takes two parallel approaches. In the first, people with TB and their contacts are identified and then treated. Identification of infections often involves testing high-risk groups for TB. In the second approach, children are vaccinated to protect them from TB. No vaccine is available that provides reliable protection for adults. However, in tropical areas where the levels of other species of mycobacteria are high, exposure to nontuberculous mycobacteria gives some protection against TB.
The World Health Organization (WHO) declared TB a global health emergency in 1993, and the Stop TB Partnership developed a Global Plan to Stop Tuberculosis that aims to save 14 million lives between 2006 and 2015 Since humans are the only host of Mycobacterium tuberculosis, eradication would be possible. This goal would be helped greatly by an effective vaccine.
Vaccines
Many countries use Bacillus Calmette-Guérin (BCG) vaccine as part of their TB control programmes, especially for infants. According to the WHO, this is the most often used vaccine worldwide, with 85% of infants in 172 countries immunized in 1993. This was the first vaccine for TB and developed at the Pasteur Institute in France between 1905 and 1921. However, mass vaccination with BCG did not start until after World War II. The protective efficacy of BCG for preventing serious forms of TB (e.g. meningitis) in children is greater than 80%; its protective efficacy for preventing pulmonary TB in adolescents and adults is variable, ranging from 0 to 80%.
In South Africa, the country with the highest prevalence of TB, BCG is given to all children under age three.prevalent; therefore BCG is not given to the entire population in these countries. In the USA, for example, BCG vaccine is not recommended except for people who meet specific criteria: However, BCG is less effective in areas where mycobacteria are less
- Infants or children with negative skin test results who are continually exposed to untreated or ineffectively treated patients or will be continually exposed to multidrug-resistant TB.
- Healthcare workers considered on an individual basis in settings in which a high percentage of MDR-TB patients has been found, transmission of MDR-TB is likely, and TB control precautions have been implemented and were not successful.
BCG provides some protection against severe forms of pediatric TB, but has been shown to be unreliable against adult pulmonary TB, which accounts for most of the disease burden worldwide. Currently, there are more cases of TB on the planet than at any other time in history and most agree there is an urgent need for a newer, more effective vaccine that would prevent all forms of TB—including drug resistant strains—in all age groups and among people with HIV.
Several new vaccines to prevent TB infection are being developed. The first recombinant tuberculosis vaccineclinical trials in the United States in 2004, sponsored by the National Institute of Allergy and Infectious Diseases (NIAID). A 2005 study showed that a DNA TB vaccine given with conventional chemotherapy can accelerate the disappearance of bacteria as well as protect against re-infection in mice; it may take four to five years to be available in humans. A very promising TB vaccine, MVA85A, is currently in phase II trials in South Africa by a group led by Oxford University, and is based on a genetically modified vaccinia virus. Many other strategies are also being used to develop novel vaccines, including both subunit vaccines (fusion molecules composed of two recombinant proteins delivered in an adjuvant) such as Hybrid-1, HyVac4 or M72, and recombinant adenoviruses such as Ad35. Some of these vaccines can be effectively administered without needles, making them preferable for areas where HIV is very common. All of these vaccines have been successfully tested in humans and are now in extended testing in TB-endemic regions. To encourage further discovery, researchers and policymakers are promoting new economic models of vaccine development including prizes, tax incentives and advance market commitments. rBCG30, entered
Screening
Mantoux tuberculin skin tests are often used for routine screening of high risk individuals.[78]
Interferon-γ release assays are blood tests used in the diagnosis of some infectious diseases. There are currently two interferon-γ release assays available for the diagnosis of tuberculosis:
- QuantiFERON-TB Gold (licensed in US, Europe and Japan); and
- T-SPOT.TB, a form of ELISPOT (licensed in Europe).
Chest photofluorography has been used in the past for mass screening for tuberculosis.
Treatment
Main article: Tuberculosis treatment
Treatment for TB uses antibiotics to kill the bacteria. Effective TB treatment is difficult, due to the unusual structure and chemical composition of the mycobacterial cell wall, which makes many antibiotics ineffective and hinders the entry of drugs. The two antibiotics most commonly used are rifampicin and isoniazid. However, instead of the short course of antibiotics typically used to cure other bacterial infections, TB requires much longer periods of treatment (around 6 to 24 months) to entirely eliminate mycobacteria from the body.Latent TB treatment usually uses a single antibiotic, while active TB disease is best treated with combinations of several antibiotics, to reduce the risk of the bacteria developing antibiotic resistance. People with latent infections are treated to prevent them from progressing to active TB disease later in life.
Drug resistant tuberculosis is transmitted in the same way as regular TB. Primary resistance occurs in persons who are infected with a resistant strain of TB. A patient with fully susceptible TB develops secondary resistance (acquired resistance) during TB therapy because of inadequate treatment, not taking the prescribed regimen appropriately, or using low quality medication. Drug-resistant TB is a public health issue in many developing countries, as treatment is longer and requires more expensive drugs. Multi-drug-resistant tuberculosis (MDR-TB) is defined as resistance to the two most effective first-line TB drugs: rifampicin and isoniazid. Extensively drug-resistant TB (XDR-TB) is also resistant to three or more of the six classes of second-line drugs.
The DOTS (Directly Observed Treatment Short-course) strategy of tuberculosis treatment recommended by WHO was based on clinical trials done in the 1970s by Tuberculosis Research Centre, Chennai, India. The country in which a person with TB lives can determine what treatment they receive. This is because multidrug-resistant tuberculosis is resistant to most first-line medications, the use second-line antituberculosis medications is necessary to cure the patient. However, the price of these medications is high; thus poor people in the developing world have no or limited access to these treatments.



Normally I wouldn’t comment on posts but I felt that I had to as your writing style is really good. You have broken down a difficult area so that it easy to understand.
ReplyDeleteThere is a safe & effective Natural Herbal Medicine. For Total Cure Call +2348142454860, or email him drrealakhigbe@gmail.com For an Appointment with (Dr.) AKHIGBE contact him. Treatment with Natural Herbal Cure. Treatment with Natural Herbal Cure For: Painful or Irregular Menstruation. HIV/Aids. Diabetics. Vaginal Infections. Vaginal Discharge. Itching Of the Private Part. Breast Infection. Discharge from Breast. Breast Pain & Itching. Lower Abdominal Pain. No Periods or Periods Suddenly Stop. Women Sexual Problems. Chronic Disease. Pain during Sex inside the Pelvis. Pain during Urination. Pelvic Inflammatory Disease, (PID). Dripping Of Sperm from the Vagina As Well As for Low sperm count. Parkinson disease. Lupus. Cancer. Tuberculosis. Zero sperm count. Asthma. Quick Ejaculation. Premature Ejaculation. Herpes. Joint Pain. Stroke. Weak Erection. Discharge from Penis. STD. Staphylococcus + Gonorrhea + Syphilis. Heart Disease. Pile-Hemorrhoid. Waist & Back Pain. Male Infertility and Female Infertility. Etc. Take Action Now. contact him & Order for your Natural Herbal Medicine: +2348142454860 and email him drrealakhigbe@gmail.com Note For an Appointment with (Dr.) AKHIGBE.I suffered in Cancer for a year and three months dieing in pain and full of heart break. One day I was searching through the internet and I came across a testimony herpes cure by doctor Akhigbe. So I contact him to try my luck, we talk and he send me the medicine through courier service and with instructions on how to be drinking it.To my greatest surprise drinking the herbal medicine within three weeks I got the changes and I was cure totally. I don't really know how it happen but there is power in Dr Akhigbe herbal medicine. He is a good herbalist doctor.
ReplyDeleteMy name is hoover, my 18 year old daughter, Tricia was diagnosed with herpes 3 years ago. Since then, we have moved from one hospital to another. We tried all kinds of pills, but every effort to get rid of the virus was futile. The bubbles continued to reappear after a few months. My daughter was using 200mg acyclovir pills. 2 tablets every 6 hours and 15g of fusitin cream. and H5 POT. Permanganate with water to be applied twice a day, but all still do not show results. So, I was on the internet a few months ago, to look for other ways to save my only son. Only then did I come across a comment about the herbal treatment of Dr Imoloa and decided to give it a try. I contacted him and he prepared some herbs and sent them, along with guidance on how to use them via the DHL courier service. my daughter used it as directed by dr imoloa and in less than 14 days, my daughter recovered her health. You should contact dr imoloa today directly at his email address for any type of health problem; lupus disease, mouth ulcer, mouth cancer, body pain, fever, hepatitis ABC, syphilis, diarrhea, HIV / AIDS, Huntington's disease, back acne, chronic kidney failure, addison's disease, chronic pain, Crohn's pain, cystic fibrosis, fibromyalgia, inflammatory Bowel disease, fungal nail disease, Lyme disease, Celia disease, Lymphoma, Major depression, Malignant melanoma, Mania, Melorheostosis, Meniere's disease, Mucopolysaccharidosis, Multiple sclerosis, Muscular dystrophy, Rheumatoid arthritis Alzheimer's disease, parkinson's disease, vaginal cancer, epilepsy Anxiety Disorders, Autoimmune Disease, Back Pain, Back Sprain, Bipolar Disorder, Brain Tumor, Malignant, Bruxism, Bulimia, Cervical Disc Disease, Cardiovascular Disease, Neoplasms , chronic respiratory disease, mental and behavioral disorder, Cystic Fibrosis, Hypertension, Diabetes, Asthma, Autoimmune inflammatory media arthritis ed. chronic kidney disease, inflammatory joint disease, impotence, alcohol spectrum feta, dysthymic disorder, eczema, tuberculosis, chronic fatigue syndrome, constipation, inflammatory bowel disease. and many more; contact him at drimolaherbalmademedicine@gmail.com./ also with whatssap- + 2347081986098.
ReplyDeleteI have being on blog Sites for a while now and today I felt like I should share my story because I was a victim too. I had HIV for 6 years and i never thought I would ever get a cure I had and this made it impossible for me to get married to the man I was supposed to get married to even after 2 years of relationship he broke up with me when he finds out I was HIV positive. So I got to know about Dr. Itua on Blog Site who treated someone and the person shared a story of how she got a cured and let her contact details, I contacted Dr. Itua and he actually confirmed it and I decided to give a try too and use his herbal medicine that was how my burden ended completely. My son will be 2 soon and I am grateful to God and thankful to his medicine too.Dr Itua Can As Well Cure The Following Disease…Alzheimer’s disease,Bechet’s disease,Crohn’s disease,Parkinson's disease,Schizophrenia,Lung Cancer,Breast Cancer,Colo-Rectal Cancer,Blood Cancer,Prostate Cancer,siva.Fatal Familial Insomnia Factor V Leiden Mutation ,Epilepsy Dupuytren's disease,Desmoplastic small-round-cell tumor Diabetes ,Coeliac disease,Creutzfeldt–Jakob disease,Cerebral Amyloid Angiopathy, Ataxia,Arthritis,Amyotrophic Lateral Scoliosis,Fibromyalgia,Fluoroquinolone Toxicity
ReplyDeleteSyndrome Fibrodysplasia Ossificans ProgresSclerosis,Seizures,Alzheimer's disease,Adrenocortical carcinoma.Asthma,Allergic diseases.Hiv_ Aids,Herpe ,Copd,Glaucoma., Cataracts,Macular degeneration,Cardiovascular disease,Lung disease.Enlarged prostate,Osteoporosis.Alzheimer's disease,
Dementia.Lupus.
,Cushing’s disease,Heart failure,Multiple Sclerosis,Hypertension,Colo_Rectal Cancer,Lyme Disease,Blood Cancer,Brain Cancer,Breast Cancer,Lung Cancer,Kidney Cancer, HIV, Herpes,Hepatitis B, Liver Inflammatory,Diabetes,Fibroid, Get Your Ex Back, If you have (A just reach him on drituaherbalcenter@gmail.com Or Whatsapp Number.+2348149277967)He can also advise you on how to handle some marital's issues. He's a good man.